Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is one of the most common complaints in the western world. Around 50% of all gastrointestinal complaints and half of all GP referrals are due to IBS. Irritable bowel syndrome is also known by many other names, such as spastic colon, mucous colitis, functional bowel disorder, dyspeptic diarrhoea, spastic constipation, anxiety and GI syndrome, and nervous bowel.
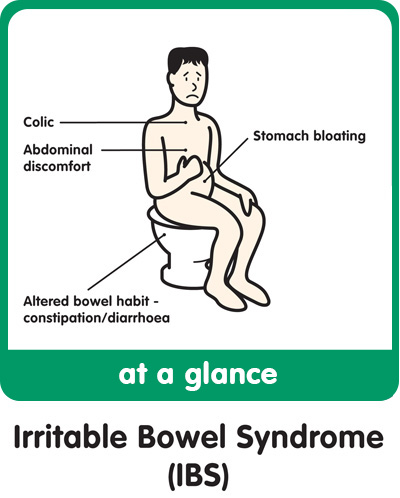
It affects 24% of all women and 19% of all men, usually developing in late adolescence or early adulthood. Before the menopause, more women than men present with IBS; after the menopause the numbers are about equal. The condition is characterized by intermittent periods of constipation or diarrhoea, often accompanied by bloating and/or abdominal pain, mucous in stools and bowel rumbling.
Irritable bowel syndrome needs to be distinguished from conditions with similar symptoms such as celiac, colorectal cancer, infective diarrhoea, diverticular disease, carcinoid syndrome, gallstones, appendicitis and inflammatory bowel disease (IBD).
Stool tests usually find nothing significant – no blood, excess white cells, parasites or bacteria. Once partly digested food has left the stomach, it is moved through the digestive tract by rhythmic contractions of the muscles in the intestinal walls, a process called peristalsis. In irritable bowel syndrome, these muscles go into spasm for unknown reasons, becoming so uncoordinated that they move residues either too quickly (causing diarrhoea) or too slowly (causing constipation).
Although IBS is often very uncomfortable, inconvenient and sometimes quite painful, (and I suffered from it for 35 years), thankfully this digestive disorder is not at all dangerous or life threatening. Nor does it ever lead to anything more “serious,” like colon cancer or ulcerative colitis.
For doctors, IBS can be challenging to diagnose, because tests often show no abnormalities even though symptoms are often all too real. As a result, a diagnosis of irritable bowel syndrome is usually arrived at by process of elimination, if you will excuse the pun, after other disorders with similar but more serious symptoms–such as diverticulitis, ulcerative colitis, Crohn’s disease, or intestinal parasites–have been ruled out.
There is no inflammation of the bowel, yet the patient suffers a variety of symptoms. These can be varying degrees of abdominal pain from vague to excruciatingly sharp; alternating constipation to diarrhoea, watery stools, wind, bloating, nausea, sweats and a worsening of symptoms after eating a large meal, during or just before menstrual periods, or while under stress.
While experts have suggested many potential causes for irritable bowel syndrome, no single cause has been established beyond a reasonable doubt. The list of possible culprits has ranged from parasitic infections and lactose intolerance, to food allergies and overuse of antibiotics.
Does any of this sound familiar? It is a good idea to rule out any serious illness, especially if you have rectal bleeding, black or mucousy stools. If you have, check with your doctor.
Some GP’s will prescribe a high bran intake for IBS sufferers, but this may be one of the worst things to do, as bran is particularly irritating to the gut. Because no two people are alike, a notion known as biochemical individuality, there is no single best diet for IBS.
It may be wise to rule out the common sensitivities and allergies to wheat, sugar, cow’s milk, beef, pork, corn, coffee and orange juice as these are the major culprits in the onset of irritable bowel syndrome. As with ulcerative colitis and Crohn’s, the ‘Stone age’ or elemental diet may help. This diet is free of all dairy, grains, red meat, refined sugars and processed foods. This can give your gut a rest from allergens and proteins that cause problems.
There are three main classifications for IBS – constipation predominate; diarrhoea predominant; and constipation/diarrhoea predominant.
Constipation predominant:
This type of IBS can be due to lack of fluid and fibre, as well as movement and exercise. Dysbiosis due to pathogens amy also be a factor.
Fibre can be added to the diet in small amounts and built up slowly. Always increase fluid intake at the same time.
Bentonite clay can also be used, as can magnesium citrate or oxide.
Diarrhoea predominant:
Factors can include lactose intolerance; food allergy or sensitivity; infective microbes.
Lactose can be eliminated from the diet by avoiding dairy products; or alternatively one can use digestive enzymes specific to the breaking down of lactose and dairy proteins.
Probiotics and Lactoferrin can help to deal with microbes that may be lurking and causing a problem.
Elimination diets can help to avoid trigger foods.
Showing all 9 results
-

Custom Probiotics 11 Strain Probiotic Powder 100g
£165.00 Add to cart -

Custom Probiotics 6 Strain Probiotic Powder
£134.00 Read more -
Custom Probiotics Acidophilus probiotic powder 50g
£60.00 Add to cart -

Custom Probiotics Four Strain Lactobacillus probiotic powder 50g
£81.00 Add to cart -
Custom Probiotics Infant Probiotic Formula 50g
£82.00 Add to cart -
Custom Probiotics L. rhamnosus powder 50g
£59.95 Read more -

Detox Support Formula
£38.99 Add to cart -
Immunecare Colostrum Super – Now 50% stronger
£29.95 Add to cart -

Immunecare Lactoferrin (Apo Lactoferrin) 90 caps
Sale! £69.95 Add to cart
Showing all 9 results